Inpatient Hospital And Limited Skilled Nursing Services Are Covered By Which Part Of Medicare?
There are some specific Medicare coverage guidelines that pertain to Skilled Nursing Facility services. Skilled nursing services are specific skills that are provided by health care employees like concrete therapists, nursing staff, pathologists, and physical therapists. Guidelines include doctor ordered care with certified health intendance employees. Also, they must treat current conditions or whatsoever new condition that occurs during your stay at a Skilled Nursing Facility. Below, we'll become over what you need to know near Medicare coverage for Skilled Nursing Facilities.
Medicare Coverage Requirements for Skilled Nursing Facilities
At that place are specific requirements that beneficiaries must meet to qualify for Medicare coverage for Skilled Nursing Facilities. The patient must have been an inpatient of a hospital facility for a minimum of 3 consecutive days. The patient must go to a Skilled Nursing Facility that has a Medicare certification within thirty days of their hospital discharge.
three Day Hosptial Stay Rule with Medicare Billing for Coverage in Skilled Nursing Facilities
For a beneficiary to extend healthcare services through SNF's, the patients must undergo the 3-day rule earlier admission. The three-day rule ensures that the beneficiary has a medically necessary stay of 3 consecutive days as an inpatient in a hospital facility. This doesn't include the 24-hour interval of the patient'south discharge, any outpatient observations, or the fourth dimension spent in the emergency room.
Exceptions to Medicare 3 Twenty-four hours Hosptial Stay Rule
If the patient'southward health conditions are non advisable for placing into a nursing facility direct after leaving the hospital, the infirmary will determine when to begin appropriate intendance. Another exception to this rule is if the patient requires around the clock nursing services.
How Long Medicare Pays for Skilled Nursing Care?
 Part A benefits cover 20 days of intendance in a Skilled Nursing Facility.
Part A benefits cover 20 days of intendance in a Skilled Nursing Facility.
After that point, Part A will encompass an boosted 80 days with the beneficiary's assistance in paying their coinsurance for every day.
Once the 100-day marker hits, a beneficiary'south Skilled Nursing Facility benefits are "exhausted".
At this bespeak, the beneficiary volition have to presume all costs of intendance, except for some Part B wellness services.
What is the Benefit Period for Skilled Nursing Facility with Medicare?
Benefit periods are how Skilled Nursing Facility coverage is measured. These periods begin on the day that the beneficiary is in the healthcare facility on an inpatient basis. This period ends when the beneficiary is no longer an inpatient and hasn't been one for sixty consecutive days.
A new do good period may begin once the prior benefit menstruation ends, and the beneficiary receives another admission to a healthcare facility. I keynote to recall is that a new benefit period is non each calendar year or change to the patient'south diagnosis or health condition.
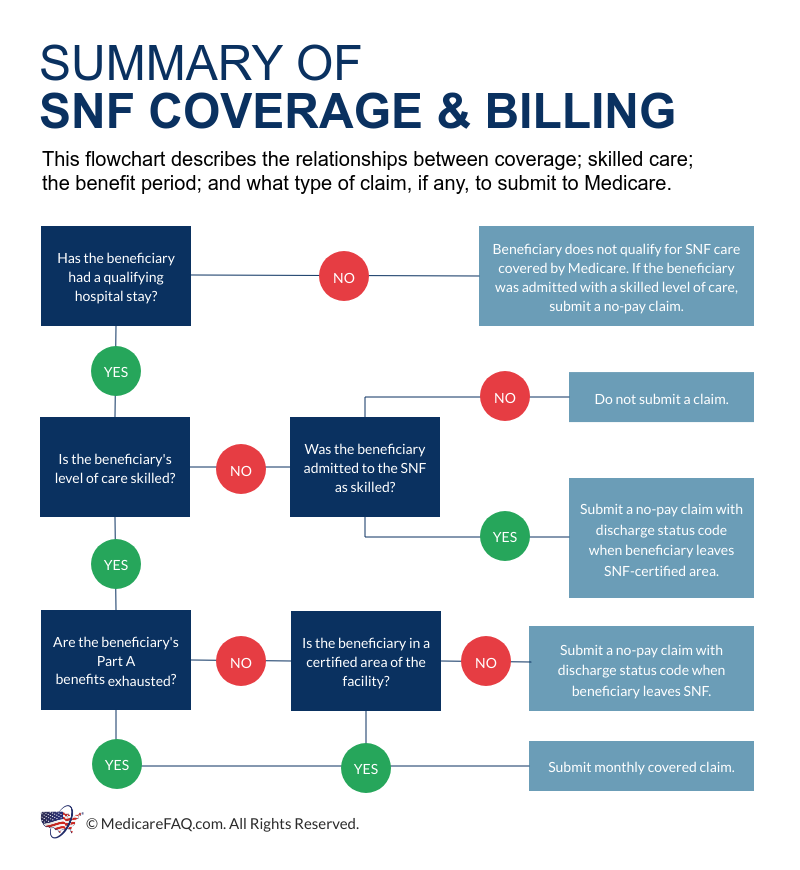
Unique Skilled Nursing Facility Billing Situations
There are instances where Medicare may require a merits, even when payment isn't a requirement.
Readmission Inside xxx Days
When the beneficiary is discharged from a skilled nursing facility, and and so readmitted within 30 days, this is considered readmission. Another case of readmission is if a beneficiary were to be in the intendance of a Skilled Nursing Facility and so ended up needing new care inside 30 days post the first noncoverage twenty-four hour period.
Exhausting Benefits
If a patient exhausts benefits, the monthly bills continue with normal submission; although, the beneficiary must however be in a Medicare facility. Full exhausted benefits mean that the beneficiary doesn't take any available days on their claim. Partially exhausted benefits mean that the beneficiary had several available benefit days on their claims.
No Payment Billing
No payment billing happens when a patient moves to a non-SNF care level and is in a Medicare facility.
Expediting Review Results for Beneficiaries
Expediting the determination processes can happen when providers initiate discharge from SNF's because of coverage reasons. Although, beneficiaries tin entreatment health service terminations through this process.
Noncovered Days
Skilled Nursing Facility requirements must exist met to obtain benefits.
Billing Situations Amongst Other Facilities
If a beneficiary needs a Skilled Nursing Facility and goes just doesn't have a qualifying stay in a infirmary facility, they can movement to a Skilled Nursing Facility after they remain for the night. They'll and then go the side by side nighttime and receive coverage.
FAQs
- Was this article helpful ?
- Yes (22)No
How to Go Help with Medicare Coverage for Skilled Nursing Facilities
If you or a loved ane needs assistance covering out-of-pocket medical expenses that Medicare doesn't cover, we can help. Contact our agents today for a free quote on supplemental options available in your area, or you can fill out our supplemental rate course to encounter your options now.
Enter your cypher code to pull plan options available in your area.
Select which Medicare plans y'all would like to compare in your expanse.
Compare rates side by side with plans & carriers bachelor in your area.
Inpatient Hospital And Limited Skilled Nursing Services Are Covered By Which Part Of Medicare?,
Source: https://www.medicarefaq.com/faqs/medicare-coverage-for-skilled-nursing-facilities/
Posted by: conklingreirrom.blogspot.com


0 Response to "Inpatient Hospital And Limited Skilled Nursing Services Are Covered By Which Part Of Medicare?"
Post a Comment